On this page
TRU-Pain: Technology Resources to better Understand Pain is an interdisciplinary project involving a collaboration between Wright State University and Duke University. The aim of this project is to develop a multi-model designed computational model to forecast pain change for individual patients and provide optimal treatment recommendations.
Overview
1.1 Motivation and Background
Sickle cell disease (SCD) is a lifelong inherited red blood cell disorders. In SCD, red blood cells become adherent and dehydrated, as well as sickle-shaped when deoxygenated, causing them to clump together and stick to blood vessel walls [1]. These processes decrease blood flow and lead to frequent vaso-occlusive painful episodes and chronic organ damage [2]. The vaso-occlusive crisis is also one of the primary reasons for emergency department visits and hospitalization in patients with SCD [3]. The treatment of SCD is palliative and mainly includes pain control, preventing infection, and preventing complications.
SCD is very costly due to a disproportionately high use of healthcare resources, as indexed by number of Emergency Department (ED) visits, hospitalizations, and days hospitalized each year [4-5]. The combined financial impact of both emergency department and hospital utilization charges for SCD has been estimated at $2.4 billion annually [6]. Potentially preventable readmissions from all diagnoses, including SCD crisis, is likely to cost Medicare alone an estimated $12 billion per year. With approximately 100,000 patients with SCD in the US, the financial burden of this chronic disease is striking.
Mobile health (mHealth) technology is well suited to management of chronic illness. A large number of mHealth systems have been widely and successfully applied to aid in patient self-management for chronic diseases or symptoms. They are usually based on smartphones and require patients to actively self-report their symptoms and activities. These active approaches have advantages in collecting subjective data and also providing communication between patients and healthcare providers. More recently, wearable sensor-based health monitoring system are experiencing rapid growth, motivated by increasing healthcare costs and the possibility of generating personalized health management strategies [7]. These systems can provide continuous passive all-day and any-place health, mental and activity status monitoring, which enable the realization of better treatment of patients and personal health management. A hybrid approach that combines both active self-reporting and passive sensor monitoring would be a superior system for pain management, however, such a hybrid system has not been found applied in the area of pain care yet [8]. The combination of mobile phones and wearable sensors provides a unique opportunity for the development of health IT intervention designed specifically for SCD, aimed at improving self-management as well as improved personalized therapy.
1.2 Health IT Intervention
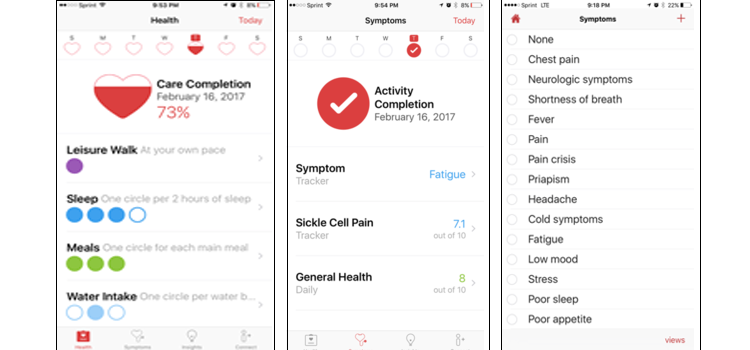
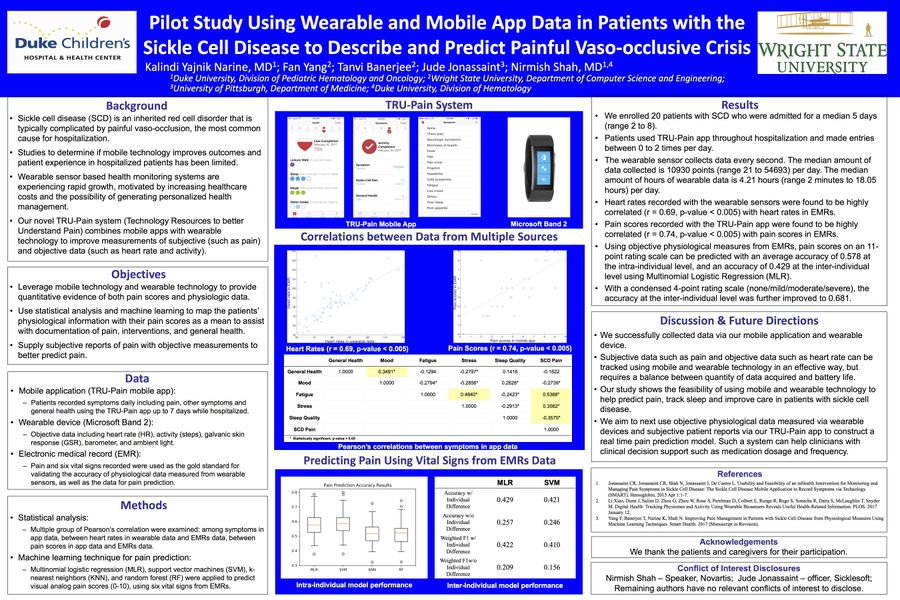
Previous studies have shown the usefulness of a SCD specific mobile application. Developed at Duke University by Dr. Nirmish Shah, pilot studies have revealed feasibility and usability of a self-developed mobile app for recording symptoms and treatment [9-10]. The mobile app is then newly revised, and functions of the TRU-Pain app are as shown in Figure 1. Patients use the app to record symptoms including pain and overall health conditions, which serves as the active approach for pain management.
For the passive approach, we utilized data from a wrist worn wearable, the Microsoft Band 2, which permits notification delivery with sound or haptic alerts based on a vast array of biological and contextual data it collects. This includes heart rate, activity, and galvanic skin response, as well as numerous other measurements such as three-axis movement, acceleration, calories, skin temperature, and ambient temperature. The band, unlike many wearable devices on the market allows developers to program apps to collect minute-by- minute data securely and directly from the device without the need for a third-party vendor accessing the data. That is important for flexibility in choice of data to collect and for security and privacy by removing third party access to data.
Right now, we have 16 patients enrolled in the study, using the app for up to 9 days while hospitalized for acute pain, with TRU-pain app data, wearable data, electronic health records and nursing records accessible for data analysis. Also, we admitted 26 patients who presented to the Duke University Adult Day Hospital for pain treatment. For this cohort, they were asked to record all symptoms including pain into the TRU-pain app and fitted with the Microsoft Band 2 during their visits in average lasting for 4.76 hours. We also working on enrolling more patients into the project.
1.3 Multi-model Forecasts
Machine learning, mathematical modeling and statistics represent fields that have contributed a large number of important tools for describing, understanding and predicting the world around us. Relatively recently all of these model types have been adopted in medicine and public health for understanding the ontogeny of diseases and managing them. However, wearable technology with an associated real-time pain forecast model is lacking. We propose the development and construction of a mathematical and computational model to make real-time forecasts based on the measured physiological biomarkers for continuous real-time pain management. Importantly, this model-integrated technology can be used simultaneously with the app to give patients and physicians real-time data recommendations for drug administration.
The broad objective of this study is to combine data from the developed app for SCD patients and the multitude of other data that are collected for these patients. Thus, the general objective is to develop individualized pain forecast models and a model-integrated sensor for optimal pain management. The in-series modeling effort that is proposed here to achieve this objective aims to decrease the size of data used in the forecasting of pain, as well as to understand the relationships between multimodal patient data including electronic health records, physiological data from the wearable sensors, and other data available to the clinicians. By doing so, personalized medical interventions can be designed based on the understanding of common population trends as well as specific individual features.
The specific objectives of this study are (1) the use of statistical and machine learning models to infer predictors of pain from big data gathered from patients and to formulate a predictive function to be used by an early warning forecast mechanistic mathematical model; (2) the development of a novel mechanistic mathematical model for pain forecast generation and a simplified model to embed into a sensor; and (3) determination of optimal drug administration and design of a forecast model-integrated sensor embedded into a wearable technology.
People
Mentors
Dr. Tanvi Banerjee (Kno.e.sis, Wright State University
Nirmish R. Shah, MD (Duke University)
Dr. Daniel M. Abrams (Northwestern University)
Researchers
Kalindi Narine, MD (Duke University Medical Center)
Amanda Johnson, MD (Duke University)
Graduate Students
Fan Yang (Kno.e.sis, Wright State University)
Shufa Khizra (Kno.e.sis, Wright State University)
Related Talks & Presentations
Publications
[1] Yang, F., Banerjee, T., Narine, K., & Shah, N. (2018). Improving Pain Management in Patients with Sickle Cell Disease from Physiological Measures Using Machine Learning Techniques. Smart Health.
Funding
Grant Number: 1R01AT010413-01
Principal Investigators: Daniel M. Abrams (Northwestern University), Tanvi Banerjee (Kno.e.sis, Wright State University), Nirmish R. Shah (Duke University)
Project Title: Collaborative research: Development and analysis of new mathematical and statistical models for chronic pain
Timeline: 09/13/2018 – 08/31/2019
Award Amount: $282,807
Media Coverage
By the numbers: Wright State graduate students Fan Yang and Michele Miller win first place in prestigious Datathon competition, Wright State University Newsroom, September 28, 2018.
Reference
[1] Zennadi, R., Moeller, B. J., Whalen, E. J., Batchvarova, M., Xu, K., Shan, S., ... & Telen, M. J. (2007). Epinephrine-induced activation of LW-mediated sickle cell adhesion and vaso-occlusion in vivo. Blood, 110(7), 2708-2717.
[2] Schnog, J. B., Duits, A. J., Muskiet, F. A., Ten Cate, H., Rojer, R. A., & Brandjes, D. P. (2004). Sickle cell disease; a general overview. Neth J Med, 62(10), 364-74.
[3] Yale, S. H., Nagib, N., & Guthrie, T. (2000). Approach to the vaso-occlusive crisis in adults with sickle cell disease. American Family Physician, 61(5), 1349-56.
[4] Woods, K., Karrison, T., Koshy, M., Patel, A., Friedmann, P., & Cassel, C. (1997). Hospital utilization patterns and costs for adult sickle cell patients in Illinois. Public Health Reports, 112(1), 44.
[5] Kauf, T. L., Coates, T. D., Huazhi, L., Mody‐Patel, N., & Hartzema, A. G. (2009). The cost of health care for children and adults with sickle cell disease. American journal of hematology, 84(6), 323-327.
[6] Lanzkron, S., Carroll, C. P., & Haywood, C. (2010). The burden of emergency department use for sickle‐cell disease: An analysis of the national emergency department sample database. American journal of hematology, 85(10), 797-799.
[7] Pantelopoulos, A., & Bourbakis, N. G. (2010). A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Transactions on Systems, Man, and Cybernetics, Part C (Applications and Reviews), 40(1), 1-12.
[8] Richardson, J. E., & Reid, M. C. (2013). The promises and pitfalls of leveraging mobile health technology for pain care. Pain medicine, 14(11), 1621-1626.
[9] Shah, N., Jonassaint, J., & De Castro, L. (2014). Patients welcome the sickle cell disease mobile application to record symptoms via technology (SMART). Hemoglobin, 38(2), 99-103.
[10] Jonassaint, C. R., Shah, N., Jonassaint, J., & De Castro, L. (2015). Usability and feasibility of an mHealth intervention for monitoring and managing pain symptoms in sickle cell disease: the sickle cell disease mobile application to record symptoms via technology (SMART). Hemoglobin, 39(3), 162-168.